OCD (Obsessive-Compulsive Disorder) Demystified
Obsessive-Compulsive Disorder, commonly referred to as OCD, is a mental health condition that affects a significant portion of the global population. Despite being a well-known disorder, there are still misconceptions and stigmas attached to OCD that can make it challenging for individuals to seek help and receive proper treatment. In this comprehensive article, we will delve into the intricate details of OCD, exploring its symptoms, causes, diagnosis, treatment options, and the impact it has on individuals' lives. By demystifying OCD, we aim to increase understanding and awareness of this disorder and encourage those affected by it to seek help and support.
Understanding OCD: Definition and Symptoms
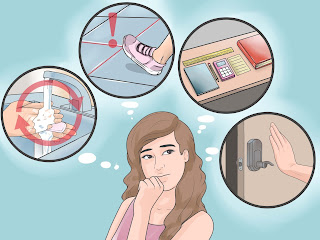
Obsessive-Compulsive Disorder is a mental health condition characterized by the presence of persistent and intrusive thoughts, images, or impulses (obsessions) that lead to repetitive behaviors or mental acts (compulsions) aimed at reducing the anxiety or distress caused by the obsessions. The hallmark features of OCD are obsessions and compulsions, and individuals may experience both or one of these components to varying degrees.
Obsessions in OCD are typically unwanted and intrusive thoughts or fears that cause significant distress or anxiety. Common obsessions include fears of contamination, fears of harming oneself or others, fears of making a mistake, and fears of losing control. These obsessions can be persistent and overwhelming, leading to feelings of anxiety, shame, and guilt. Individuals may recognize that these obsessions are irrational, but they are unable to shake off the anxiety they provoke.
Compulsions are repetitive behaviors or mental acts that individuals feel compelled to perform in response to their obsessions. Compulsions are aimed at reducing the anxiety caused by obsessions, although they only provide temporary relief. Common compulsions include excessive hand-washing or cleaning in response to fears of contamination, checking behaviors in response to fears of harm, repeating rituals in response to fears of making a mistake, and mental rituals in response to fears of losing control.
The symptoms of OCD can vary widely among individuals, and the specific obsessions and compulsions experienced may differ from person to person. Despite this variability, the underlying theme in OCD is the presence of unwanted intrusive thoughts and the need to engage in rituals to alleviate distress. The severity of symptoms can also fluctuate, with some individuals experiencing mild symptoms that are manageable, while others may struggle with severe symptoms that significantly impact their daily functioning.
Causes of OCD: Understanding the Factors
The precise causes of Obsessive-Compulsive Disorder are not fully understood, and research suggests that a combination of genetic, biological, environmental, and psychological factors may contribute to the development of the disorder. Some of the key factors believed to play a role in the etiology of OCD include:
Genetic Factors: Studies have indicated that OCD tends to run in families, suggesting a genetic predisposition to the disorder. Individuals with a family history of OCD may be at a higher risk of developing the condition themselves.
Brain Chemistry: Imbalances in neurotransmitters, such as serotonin, dopamine, and glutamate, have been implicated in the development of OCD. These chemical messengers play a crucial role in regulating mood, anxiety, and behavior, and disruptions in their levels may contribute to the symptoms of OCD.
Environmental Factors: Traumatic events, stressful life experiences, or exposure to chronic stressors may trigger the onset of OCD in some individuals. These environmental factors can play a role in the development and exacerbation of OCD symptoms.
Psychological Factors: Certain psychological traits, such as perfectionism, low self-esteem, and high levels of anxiety, may predispose individuals to the development of OCD. Individuals with OCD may have rigid thought patterns and difficulties tolerating uncertainty, which can amplify obsessions and compulsions.
Diagnosis and Evaluation of OCD
Diagnosing OCD typically involves a comprehensive evaluation by a mental health professional, such as a psychiatrist or psychologist. The diagnostic criteria for OCD are outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association. To receive a diagnosis of OCD, an individual must meet specific criteria related to the presence of obsessions and compulsions, their impact on daily functioning, and the distress or impairment they cause.
During the evaluation process, the mental health professional will conduct a thorough assessment of the individual's symptoms, medical history, and psychosocial factors. They may use standardized questionnaires, interviews, and assessments to gather information about the nature and severity of the individual's symptoms. Family history and any underlying medical or psychiatric conditions will also be considered during the evaluation process.
In some cases, additional tests, such as blood tests or neuroimaging studies, may be recommended to rule out other medical conditions that could be contributing to the symptoms. It is essential for individuals undergoing evaluation for OCD to be open and honest about their experiences and symptoms to ensure an accurate diagnosis and appropriate treatment plan.
Treatment Options for OCD: Strategies for Management
Treatment for Obsessive-Compulsive Disorder typically involves a combination of psychotherapy, medication, and lifestyle modifications aimed at reducing symptoms and improving overall quality of life. The most common treatment options for OCD include:
Cognitive-Behavioral Therapy (CBT): CBT, particularly a specialized form known as Exposure and Response Prevention (ERP), is considered the gold standard treatment for OCD. In ERP, individuals are gradually exposed to their fears or triggers while learning to resist engaging in compulsive behaviors. This exposure helps individuals confront their fears and learn to tolerate anxiety without resorting to rituals.
Medication: Antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants, are commonly prescribed to individuals with OCD. These medications can help regulate neurotransmitter levels in the brain, reducing the severity of obsessions and compulsions. It is essential to work closely with a healthcare provider to determine the most appropriate medication and dosage for each individual.
Deep Brain Stimulation (DBS): In cases of severe and treatment-resistant OCD, Deep Brain Stimulation (DBS) may be considered as a potential treatment option. DBS involves implanting electrodes in specific areas of the brain to modulate abnormal neural activity associated with OCD symptoms. While DBS is typically reserved for severe cases, it has shown promising results in reducing OCD symptoms in some individuals.
Supportive Therapies and Self-Care: In addition to formal treatments, individuals with OCD can benefit from engaging in self-care strategies and supportive therapies to manage their symptoms. Joining a support group, practicing relaxation techniques, incorporating exercise and mindfulness into daily routines, and maintaining a healthy lifestyle can all contribute to overall well-being and symptom management.
The Impact of OCD and Promoting Awareness
Obsessive-Compulsive Disorder can have a profound impact on the lives of individuals affected by the condition, as well as their family members and loved ones. The constant presence of obsessions and compulsions can lead to feelings of shame, guilt, and embarrassment, contributing to social isolation and impaired quality of life. Individuals with OCD may experience challenges in maintaining relationships, pursuing academic or career goals, and engaging in everyday activities due to the disruptive nature of their symptoms.
Furthermore, the stigma surrounding mental health conditions, including OCD, can prevent individuals from seeking help and support. Misconceptions about OCD as merely a character flaw or a personality quirk can perpetuate feelings of shame and discourage individuals from seeking treatment. It is crucial to promote awareness and understanding of OCD as a legitimate and treatable mental health disorder to reduce stigma and encourage those affected by it to seek help.
By increasing awareness of OCD and providing accurate information about the condition, we can empower individuals to recognize their symptoms, seek appropriate treatment, and engage in self-care practices that promote well-being. It is essential for mental health professionals, educators, policymakers, and the general public to work together to destigmatize OCD and create a supportive environment for individuals living with the disorder.
In conclusion, Obsessive-Compulsive Disorder is a complex and challenging mental health condition that affects individuals worldwide. By understanding the symptoms, causes, diagnosis, treatment options, and impact of OCD, we can demystify the disorder and provide support to those affected by it. It is crucial for individuals with OCD to seek help from qualified mental health professionals, engage in evidence-based treatments, and prioritize self-care strategies to manage their symptoms effectively. Through education, awareness, and advocacy, we can create a more compassionate and inclusive society that supports the well-being of individuals living with OCD.
Comments
Post a Comment